I
n a bold and unexpected move intended to combat the opioid crisis, the Kentucky Opioid Abatement Advisory Commission recently announced plans to allocate at least $42 million over the next six years to research the potential of the psychedelic compound Ibogaine for treating opioid addiction. This decision marks a significant shift in the conventional approach to addressing drug abuse and addiction, particularly in the conservative South. It also represents a notable embrace of the emerging field of psychedelic medicine.(1)
Kentucky’s funding for psychedelic medicine research comes from a recent legal win and subsequent settlement with major opioid manufacturers. It is also part of a broader effort to find innovative solutions to the opioid crisis, which claimed the lives of more than 2000 Kentuckians in 2022, and killed an estimated 79,177 Americans last year.(2, 3)
The state intends to develop what they call the “platinum standard model” for an ibogaine recovery protocol. This will be achieved through several multi-site clinical trials held within the state. Moreover, the funds will be used to foster public-private partnerships that can support and drive the development of ibogaine through the Food and Drug Administration approval process.(1)
The decision to focus on ibogaine is rooted in emerging science which indicates that ibogaine has significant potential for treating substance use disorders, especially where traditional treatment modalities have failed in the past. The Veterans Mental Health Leadership Coalition, a non-profit organization advocating for psychedelic reform and legalization, played a crucial role in organizing and briefing advocates who spoke on the paradigm-shifting potential of ibogaine.(4)
Keep Up with Uncensored Psychedelic Trends
Join our newsletter at Psychedelics Uncensored.
We respect and protect your privacy. By subscribing your info will be subject to our privacy policy . Unsubscribe easily at any time
What are Psychedelics?
Psychedelics are a class of serotonergic (meaning they impact the serotonin system) drugs that can cause profound changes in consciousness. Classical psychedelics include psilocybin (aka magic mushrooms), lysergic acid diethylamide (LSD), dimethyltryptamine (DMT), the Amazonian brew ayahuasca, and of course, ibogaine. Other non-classical psychedelics that are undergoing research as a treatment for mental health conditions include 3,4-Methylenedioxymethamphetamine (MDMA), 5-MEO-DMT, and ketamine.(5, 6)
These compounds have been used by various cultures as important medicinal and spiritual tools for millennia but have only recently gained the attention of Western medicine after decades of stigmatizing propaganda campaigns and prohibition. The potential medical uses for psychedelics are vast, with applications for conditions such as treatment-resistant depression, PTSD, anxiety, substance abuse disorders, and even end-of-life care. With this new investment into psychedelic research, Kentucky joins a growing roster of states, like Colorado, Oregon, Washington, Virginia, and Hawaii, all of whom are exploring the use of psychedelics as medicine.(7)
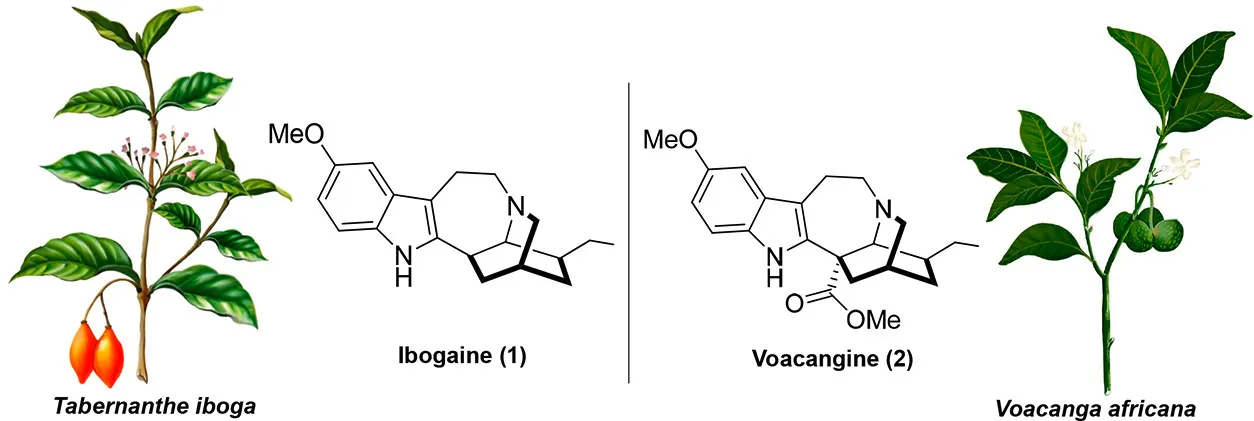
What is Ibogaine?
Ibogaine is a naturally occurring psychoactive substance found in plants in the Apocynaceae family, such as Tabernanthe iboga. It is a powerful hallucinogen with complex pharmacology, and it has been used traditionally in spiritual and healing rituals by indigenous communities in West Africa, particularly in Gabon.(8)
Ibogaine is unique among psychedelics for its reported ability to significantly reduce withdrawal symptoms and cravings associated with substance use disorders, particularly opioids. It’s also been explored as a potential treatment for addictions to other substances, including alcohol, cocaine, and methamphetamine.(8)
The mechanism by which ibogaine works is not fully understood, but it’s believed to affect various neurotransmitter systems simultaneously. Some research suggests that ibogaine affects the opioid receptors in the brain, which could explain its effects on withdrawal and cravings. It also affects other neurotransmitter systems, including those involving serotonin, dopamine, and glutamate, which could contribute to its psychedelic effects and potential therapeutic benefits.(8)
Regarding its use as a treatment for substance use disorder, ibogaine therapy usually involves a single administration of the drug in a controlled, clinical setting under the supervision of trained medical professionals. The experience can last up to 24 hours or more and is often described as intensely introspective, allowing individuals to confront experiences and emotions tied to their addiction.(8)
It’s important to note that while the potential benefits of ibogaine treatment are promising, it does come with significant risks, including cardiovascular complications and potentially life-threatening side effects. As such, it’s critical that any use of ibogaine for treating substance use disorders is carried out under medical supervision.(8)
Finally, while preliminary studies and anecdotal reports suggest that ibogaine could be an effective treatment for substance use disorders, more rigorous scientific research is needed to confirm its efficacy and safety. This is why initiatives such as the one in Kentucky are so important.(1)
Keep Up with Psychedelic Trends
Get uncensored psychedelic news, events, and updates. Join Psychedelics Uncensored!
We respect and protect your privacy. By subscribing your info will be subject to our privacy policy . Unsubscribe easily at any time
Sources

1. Kentucky Opioid Abatement Advisory Commission – Kentucky Attorney General. (n.d.). Www.ag.ky.gov. Retrieved June 1, 2023, from https://www.ag.ky.gov/Priorities/Tackling-the-Drug-Epidemic/Pages/Opioid-Abatement-Advisory-Commission-.aspx
2. Gov. Beshear: Kentucky Drug Overdose Deaths Decline for First Time in Four Years – Kentucky Justice & Public Safety Cabinet. (n.d.). Justice.ky.gov. Retrieved June 1, 2023, from https://justice.ky.gov/News/Pages/2022overdosedeathsreport.aspx
3. Overdose Deaths Declined but Remained Near Record Levels During the First Nine Months of 2022 as States Cope with Synthetic Opioids. (2023, March 13). Www.commonwealthfund.org. https://www.commonwealthfund.org/blog/2023/overdose-deaths-declined-remained-near-record-levels-during-first-nine-months-2022-states
4. Noller, G. E., Frampton, C. M., & Yazar-Klosinski, B. (2017). Ibogaine treatment outcomes for opioid dependence from a twelve-month follow-up observational study. The American Journal of Drug and Alcohol Abuse, 44(1), 37–46. https://doi.org/10.1080/00952990.2017.1310218
5. Nichols, D. E. (2016). Psychedelics. Pharmacological Reviews, 68(2), 264–355. https://doi.org/10.1124/pr.115.011478
6. Doblin, R. E., Christiansen, M., Jerome, L., & Burge, B. (2019). The Past and Future of Psychedelic Science: An Introduction to This Issue. Journal of Psychoactive Drugs, 51(2), 93–97. https://doi.org/10.1080/02791072.2019.1606472
7. Gregorio, D. D., Aguilar-Valles, A., Preller, K. H., Heifets, B. D., Hibicke, M., Mitchell, J., & Gobbi, G. (2021). Hallucinogens in Mental Health: Preclinical and Clinical Studies on LSD, Psilocybin, MDMA, and Ketamine. Journal of Neuroscience, 41(5), 891–900. https://doi.org/10.1523/JNEUROSCI.1659-20.2020
8. Ibogaine – an overview | ScienceDirect Topics. (n.d.). Www.sciencedirect.com. https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/ibogaine
This material is not intended as a replacement or substitute for any legal or medical advice. Always consult a medical professional about your health needs. Psychedelics are widely illegal in the United States, and readers should always be informed about local, state, and federal regulations regarding psychedelics or other drugs.

 David Connell
David Connell